Alicia M. Yochum, RN, DC, DACBR
Alicia M. Yochum received her Bachelor of Science in Nursing degree from Point Loma Nazarene University and DC degree from Logan College of Chiropractic, where she graduated Suma Cum Laude. She completed her imaging Residency at Logan in 2015 and received her DACBR, becoming the first second-generation DACBR in the history of chiropractic. Dr. Yochum is also RMSK certified. She has performed editorial review for the Journal of Chiropractic Medicine and she serves as an Associate Editor for the Journal of the Academy of Chiropractic Orthopedics (JACO). Dr. Yochum has published many articles in peer-reviewed journals and has lectured around the country as well as in England, Germany, Australia and New Zealand. She completed her fellowship in musculoskeletal advanced imaging at Logan University with an emphasis on musculoskeletal diagnostic ultrasound. Dr. Yochum is currently practicing at Rocky Mountain Chiropractic Radiological Center in Denver, Colorado.
INTRODUCTION
Diagnostic ultrasound is an imaging tool being increasingly utilized for the identification of musculoskeletal abnormalities, such as muscular and tendon pathology. This, along with basic ultrasound orientation, terminology and benefits will be discussed in this article, as well as the appearance of various tendon pathologies demonstrated by case examples.
Ultrasound technology was first utilized on living tissue by Wild and colleagues in 1951, and has been widely used in the medical field ever since.1 The understanding by most medical providers (and the general public) is that ultrasound is for use on organ structures such as the liver, kidneys, uterus, heart and vasculature, however it is now also being utilized to image various musculoskeletal structures. Its application is primarily in the extremities, examining ligaments, muscles, tendons, joints, cartilage and nerves.
One of the significant benefits of ultrasound imaging is the examiner’s ability to move the patient to dynamically image structures under stress. A ligament or joint can be stressed to ensure its integrity, which can even be done in a weightbearing or pain-provoking position. Muscle activation can help identify or determine the extent of the injury. Another substantial benefit of ultrasound is the ability to image blood flow (called doppler flow or hyperemia). This flow increases in an acute injury, which can be differentiated with ultrasound from a chronic injury which would not show increased blood flow. Utilizing doppler flow can help determine the age of an injury, which cannot be achieved with other imaging modalities.
Limitations in the scope of ultrasound include structures that are deep within the joint, such as the labrum or deep articular cartilage (osteochondral defect on the talar dome). This article’s focus, however, is on the imaging of muscular and tendon injury.
ACCURACY AND RESOLUTION
It was first discovered in 1980 that the appearance of normal muscle is different than that of muscle affected by pathology.2 The resolution that can be obtained while imaging the musculoskeletal (MSK) system with ultrasound is approximately 0.1 mm, which is better than using 3 Tesla-strength magnetic resonance imaging (MRI) which can obtain a resolution of 0.2 x 0.2 x 1 mm. The high resolution of ultrasound allows for a high level of accuracy in diagnosis. For example, when comparing partial and full-thickness rotator cuff tears, the sensitivity and specificity of both MRI and ultrasound is comparable, if not slightly more specific, utilizing ultrasound.3 The most sensitive and specific imaging for cuff injury is MR arthrogram, with sensitivity and specificity higher than both standard MRI and ultrasound (this, however, is more invasive).
ULTRASOUND TERMINOLOGY
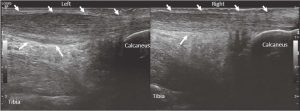
It is important to understand basic terminology regarding ultrasound when discussing the appearance of any structure. When describing the orientation of imaging, both long-axis and short-axis are utilized (these refer to the probe orientation in relation to the target structure being imaged). Long-axis refers to being aligned with the course of the structure (parallel) and short-axis refers to being aligned against the course of the structure (perpendicular). This can also be likened to MRI, with long-axis being similar to imaging in the sagittal plane in a structure such as the Achilles tendon, and short-axis being similar to the axial/transverse plane (Figures 2, 3 and 5). In all images, the top of the image is superficial with the skin at the top and then the bottom of the image usually deep with a bone landmark. In long-axis images, the left of the image is proximal or cephalic and the right of the image is distal or caudal. In short-axis images, the right is medial and left is lateral.
The other terms utilized when describing ultrasound images refer to the range on the gray scale. Hypoechoic means that there are fewer sound echoes interacting with a structure, making it appear dark grey or even close to black on the image. Hyperechoic means that there are more sound waves interacting, making the structure appear white on the image. Anechoic means an absence of wave interaction, and this term is used when referring to fluid where the sound waves move freely with no interaction with dense structures. These terms also refer to the appearance of bone. The cortex of the bone is very hyperechoic, as all of the sound waves reflect back from the bone to the transducer. These sound waves cannot penetrate the bone, producing shadowing (acoustic shadowing) or an area of no sound wave interaction (anechoic) below the cortex.
NORMAL MUSCULAR APPEARANCE
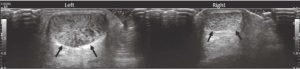
Ultrasound waves interact with anatomical structures, such as muscles and tendons, giving each one a specific appearance when imaged. In short axis, the muscle has a primarily hypoechoic/dark appearance with speckles (this is often referred to as “starry-eyed” due to the visualization of the perimysial tissue which is more hyperechoic/white). Long-axis imaging displays the linear appearance of the muscle fascicles, and this differs depending on the type of muscle imaged (i.e., parallel, bipennate, unipennate or circular).4 Tendons are denser and have a more hyperechoic fibrillar appearance in long axis. In short axis, the tendon appears hyperechoic and has been likened to bristles on a brush (Figures 2 and 3).5
One key artifact that is important to mention is that of anisotropy, which deals with the correct orientation of the probe in relation to the tendon. It is important that the probe is perpendicular to the sound waves in order to get a clear and accurate echo from the tendon. If the tendon is curving away from the probe, the sound waves do not bounce back to the probe directly and therefore are “lost,” creating an area of no sound wave interaction which can be confused with pathology. This is very common in the rotator cuff tendon, as it curves toward the greater tuberosity insertion (Figure 7).
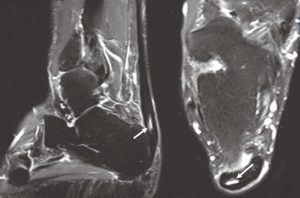
MUSCULAR AND TENDON TEARS
When a tendon or muscle tears, the most specific sign of that tear is a collection of fluid (this feature is true of both MRI and ultrasound imaging). On ultrasound, fluid has no echogenicity, creating an anechoic/very black appearance described above. This is opposite to the standard T2 MRI images that we review to confirm tearing where water is white (Figure 5). There may be variable echogenicity related to tearing due to hematoma formation or hemorrhage, which would often have heterogenous or mixed echotexture.5 The easiest type of tear to identify is a full-thickness tear, as there is complete detachment of the tendon insertion with retraction and fluid filling the gap. If there is no obvious retraction, muscle contraction and movement can be utilized to help demonstrate the extent of tearing. Partial thickness tears can be harder to identify.
The orientation of the tendon or muscle fibers is important, as a wavy or disrupted course of the fibers indicates tearing. It is imperative to localize tears in both the long and short axis the same way we confirm any imaging finding in two planes. The key features of tendinosis are thickening of the tendon with diffuse fluid within the tendon, without focal fluid that can be measured.5
Blood flow is increased in an area of tearing (hyperemia), which can indicate neovascularity, or the body’s natural attempt at healing. Doppler imaging allows the practitioner to more accurately determine if a tendon tear or injury is old (no blood flow) or new (active blood flow). Clinically, the hyperemia commonly correlates to the location of the patient’s primary region of pain or primary pain generator. MRI can accurately identify tears, but does not have the ability to determine an active area of inflammation verses an old injury the way that ultrasound can.
CASE EXAMPLES
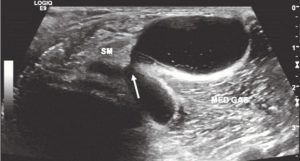
Baker Cyst
A Baker cyst demonstrates a good example of multiple echotextures observable with ultrasound. Also known as the semimembranousus (SM) medial gastrocnemius (MED GAS) bursa, a Baker cyst is a communicating bursa which means that it forms when there is a large intra-articular effusion in the knee that “leaks.” Note in Figure 1 the neck of the Baker cyst as the fluid comes out between the SM and MED GAS tendons.
Achilles Tendon
This patient’s right Achilles tendon is normal, with a fibrillar appearance in long axis (Figure 2) and a brush-on-end hyperechoic appearance in short axis (Figure 3). The left Achilles tendon is abnormal, demonstrating signs of tendinosis such as thickening (arrows) and diffuse hypoechoic echotexture, however there is no fiber disruption or fluid collections which would indicate tearing.
Tendon or muscular tearing is present when there is a fluid collection with fiber disruption (Figure 4). Partial tearing is present when a small portion of the tendon has focal fluid within that can be measured. MRI demonstrates a similar finding with a focal fluid collection within the tendon, indicating partial tearing in Figure 5.
Full-thickness Achilles tendon tearing is demonstrated in Figure 6, with more prominent disorganization of fiber orientation and a gap in the continuity of the tendon. There is also pronounced thickening of the Achilles tendon distal to the tear, which indicates that there was tendinosis prior to tearing as tendinosis is a chronic finding and can weaken the tendon. Dynamic imaging is often very useful in determining the integrity of the tendon with active and passive muscle contraction.
Rotator Cuff
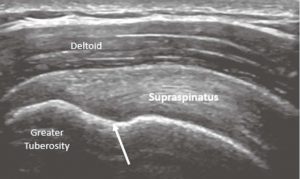
The supraspinatus tendon’s normal appearance has a curved contour deep to the deltoid, and the greater tuberosity has a notch at the insertion. It is at this notch that it is common to see anisotropy, which should not be confused with a tear (Figure 7).
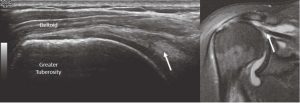
Full-thickness tearing is seen with fiber disruption, fluid collection and tendon retraction similar to full-thickness tearing in the Achilles (or any) tendon (Figure 8). The anatomy can be compared to MRI.
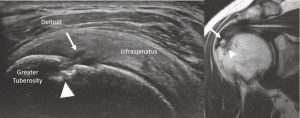
Partial tearing can be more difficult to see with a smaller area of fluid collection and fiber disruption without tendon retraction. It is common to see cortical defects deep to tendon tears as a secondary sign of tearing (Figure 9).
Rectus Femoris
Full-thickness tearing of the rectus femoris muscle often retracts proximally and presents with a palpable bump with an indentation in the quadriceps muscle. Fluid will be present in the tear, often with hematoma due to the large muscle belly tearing.
CONCLUSION
Ultrasound is a dynamic imaging modality whose usage is expanding for the musculoskeletal system. It has a high resolution and is accurate at diagnosing many injuries to the musculoskeletal system, including muscle and tendon injuries. It has the ability to be very dynamic with movement and muscle contraction, and can aid in determining the age of a lesion with doppler imaging. As its use continues to expand, it can play a vital role aiding in the diagnosis and treatment of patients.
REFERENCES
- Wild JJ, Neal D. Use of high-frequency ultrasonic waves for detecting changes of texture in living tissues. Lancet. 1951;1:655-657.
- Finanger E, Russman B, Forbes S, et al. Use of skeletal MRI in diagnosis and monitoring disease progression in Duchenne muscular dystrophy. Phys Med Rehabil Clin N Am. 2012:23 (1)1-ix.
- DeJesus J, Parker L, Frangos A, Nazarian L. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. American journal of roentgenology. 2009;192:1701-1707.
- Pillen S. Skeletal muscle ultrasound. European Journal Translational Myology. 2010;1(4)145-155.
- Jacobson J. Fundamentals of musculoskeltal ultrasound. 3rd ed. Philadelphia: Elsevier; 2018.